Pelvic fractures can be a real challenge in trauma care. They’re not just painful—they can cause life-threatening bleeding, come with other serious injuries, and sometimes lead to long-term disabilities.
To treat these injuries effectively, healthcare professionals need a solid grasp of pelvic anatomy, how fractures are classified, and the key principles of treatment.
This article dives deep into pelvic fractures—covering the anatomy, how doctors classify these injuries, what they look like in patients, and how they’re diagnosed. It also breaks down both non-surgical and surgical treatment options.
We’ll also explore possible complications and share the latest research to give medical students a complete guide to this complex topic.
Anatomy and Biomechanics of the Pelvis
The pelvis is a complex structure that serves as the foundation for the trunk and lower extremities.
It plays a critical role in weight-bearing, locomotion, and protection of vital organs.
Understanding the intricate anatomy and biomechanics of the pelvis is essential for comprehending the mechanisms and patterns of pelvic fractures.
Bony Structures
The pelvic girdle is formed by two innominate bones (hip bones) that articulate with the sacrum posteriorly. Each innominate bone is composed of three fused bones: the ilium, ischium, and pubis.
Ilium: The ilium is the largest and most superior of the three pelvic bones.
It forms the prominence of the hip and provides attachment for numerous muscles, including the gluteal muscles and the iliopsoas.
The iliac crest is the superior border of the ilium and serves as an important landmark for physical examination and surgical approaches.
The ilium articulates with the sacrum at the sacroiliac joint.
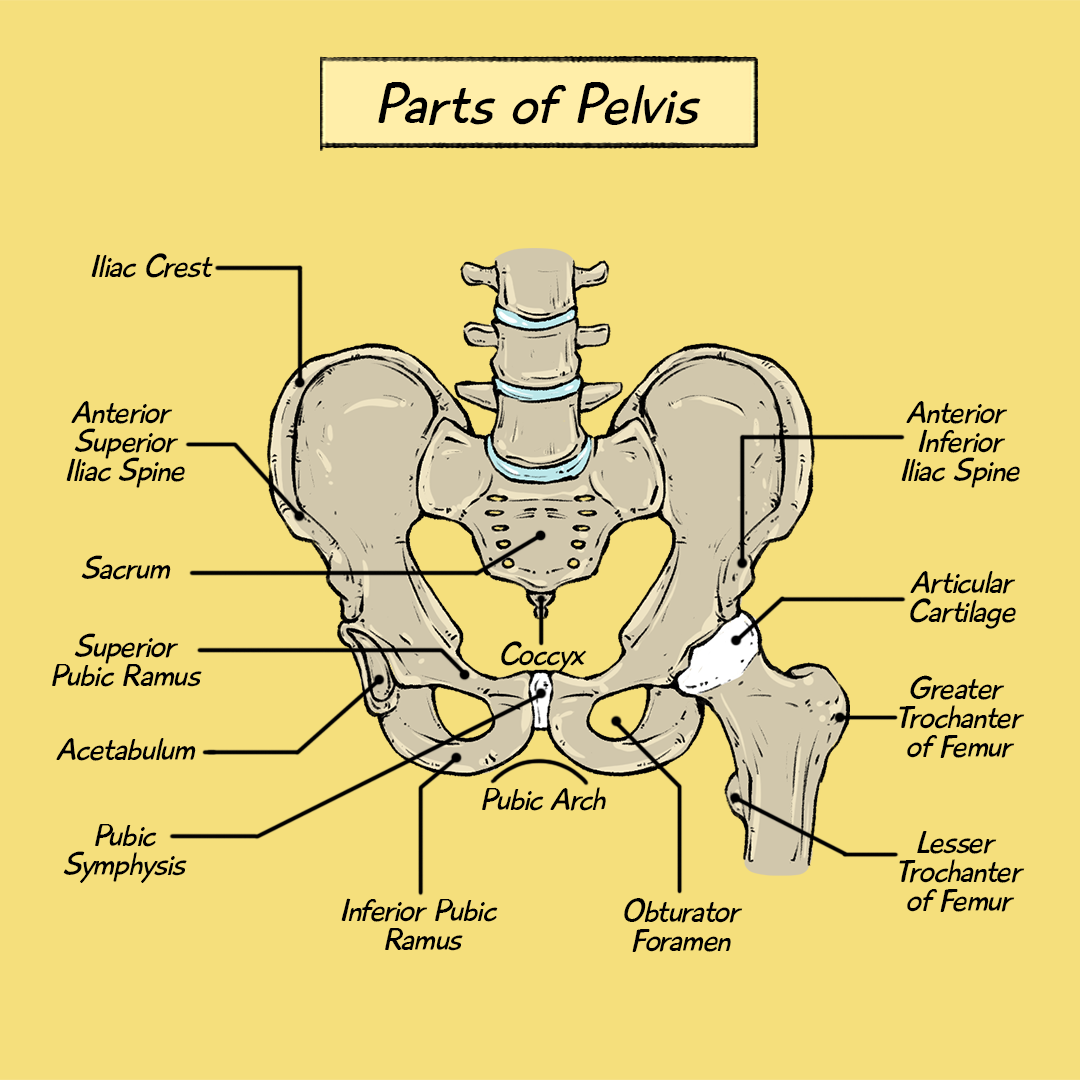
Ischium: The ischium forms the posteroinferior portion of the hip bone. It provides support for the body when sitting and serves as the origin for hamstring muscles.
The ischial tuberosity is a prominent bony projection on the inferior aspect of the ischium.
The ischium also contributes to the formation of the obturator foramen, a large opening in the pelvis.
Pubis: The pubis forms the anteroinferior portion of the hip bone.
The two pubic bones meet anteriorly at the pubic symphysis, a fibrocartilaginous joint.
The pubis provides attachment for muscles of the abdominal wall and the medial thigh.
These three bones fuse together at the acetabulum, a cup-shaped socket that articulates with the head of the femur to form the hip joint.
Articulations
Sacroiliac Joints: The sacroiliac joints are strong, synovial joints that connect the sacrum to the ilium on each side.
They are essential for stability of the pelvis and transmit forces between the spine and lower extremities.
The sacroiliac joints are reinforced by strong ligaments, including the anterior, posterior, and interosseous sacroiliac ligaments.
Pubic Symphysis: The pubic symphysis is a cartilaginous joint that connects the two pubic bones anteriorly.
It allows for slight movement during activities such as walking and childbirth.
The pubic symphysis is supported by the superior and inferior pubic ligaments.
Ligamentous Support
Ligaments are strong, fibrous bands that connect bones and provide stability to joints.
The pelvis is stabilized by a complex network of ligaments, which play a crucial role in maintaining its integrity and resisting external forces.
Sacroiliac Ligaments: The sacroiliac ligaments are among the strongest ligaments in the body.
They provide significant stability to the sacroiliac joints, preventing excessive movement and displacement.
The posterior sacroiliac ligaments are particularly important in resisting rotational forces.
Sacrotuberous and Sacrospinous Ligaments: These ligaments connect the sacrum to the ischial tuberosity and ischial spine, respectively.
They contribute to pelvic stability and prevent excessive rotation of the sacrum.
Iliolumbar Ligaments: The iliolumbar ligaments connect the ilium to the lumbar vertebrae.
They help to stabilize the lumbosacral junction and transmit forces between the spine and pelvis.
Inguinal Ligament: While not directly involved in pelvic stability, the inguinal ligament is an important anatomical landmark in the groin region.
It forms the floor of the inguinal canal, through which the spermatic cord in males and the round ligament in females pass.
Mechanisms of Injury
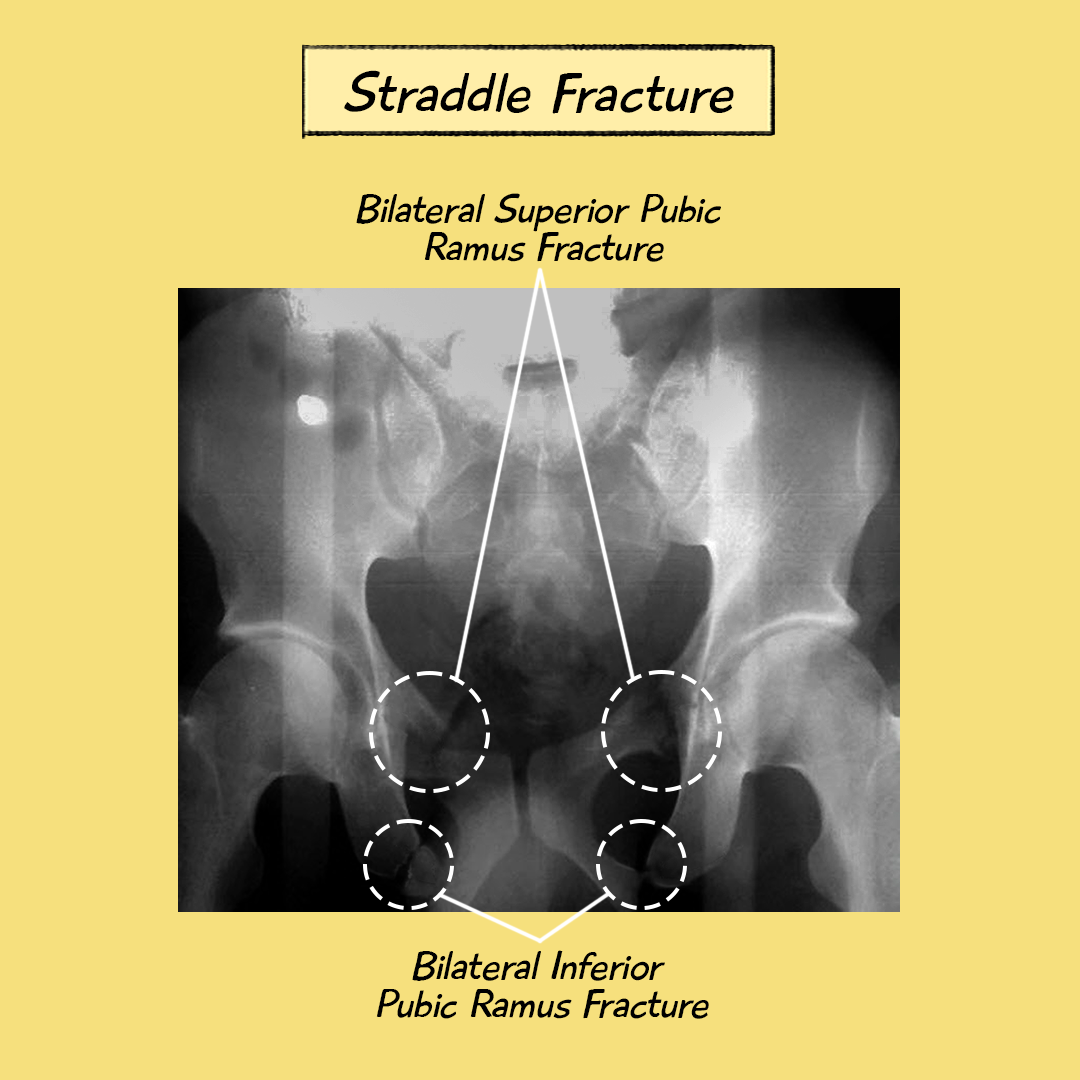
Lateral Compression (LC): Lateral compression forces, often seen in side-impact motor vehicle accidents, typically result in fractures of the pubic rami and the ilium.
The degree of instability increases with the severity of the lateral compression force.
Anteroposterior Compression (APC): Anteroposterior compression forces, such as those experienced in head-on collisions or falls onto the buttocks, can cause open-book fractures, where the pubic symphysis separates.
These forces can also disrupt the sacroiliac joints and posterior ligaments.
Vertical Shear (VS): Vertical shear forces, commonly seen in falls from heights, can cause vertical displacement of one hemipelvis relative to the other.
These injuries are often associated with significant ligamentous disruption and instability.
Combined Mechanism: Many pelvic fractures involve a combination of these forces, resulting in complex fracture patterns and significant instability.
Based on the mechanism of injury, pelvic fractures can be classified into different types.
Classification of Pelvic Fractures
Classifying pelvic fractures is essential for guiding treatment decisions, predicting potential complications, and communicating effectively among healthcare providers.
Several classification systems have been developed, each with its own strengths and limitations.
Young-Burgess Classification
The Young-Burgess classification system is widely used and is based on the mechanism of injury.
It categorizes pelvic fractures into four main types: lateral compression (LC), anteroposterior compression (APC), vertical shear (VS), and combined mechanism.
Tile Classification
The Tile classification system categorizes pelvic fractures based on their stability.
- Type A: Stable fractures. These fractures are minimally displaced and do not disrupt the pelvic ring. They are generally treated non-operatively.

- Type B: Rotationally unstable but vertically stable fractures. These fractures involve disruption of the anterior pelvic ring, such as open-book fractures. They may require external fixation or internal fixation.
https://cdn.geckomed.ai/resources/511e9fd0-822f-11ef-b4e6-3f15e55a88ab
- Type C: Rotationally and vertically unstable fractures. These fractures involve disruption of both the anterior and posterior pelvic rings. They are often associated with significant hemorrhage and require aggressive management.
https://cdn.geckomed.ai/resources/75139cd0-8232-11ef-b4e6-3f15e55a88ab
Recognizing the clinical presentation and accurately assessing the severity of a pelvic fracture are crucial for appropriate management.
Clinical Presentation and Assessment of Pelvic Fracture
Patients with pelvic fractures may present with various symptoms, including pain, shock, and difficulty urinating.
A thorough physical examination and imaging studies are essential for accurate diagnosis and assessment of the injury.
Imaging Studies
Imaging studies are essential for confirming the diagnosis of a pelvic fracture, classifying the fracture, and identifying associated injuries.
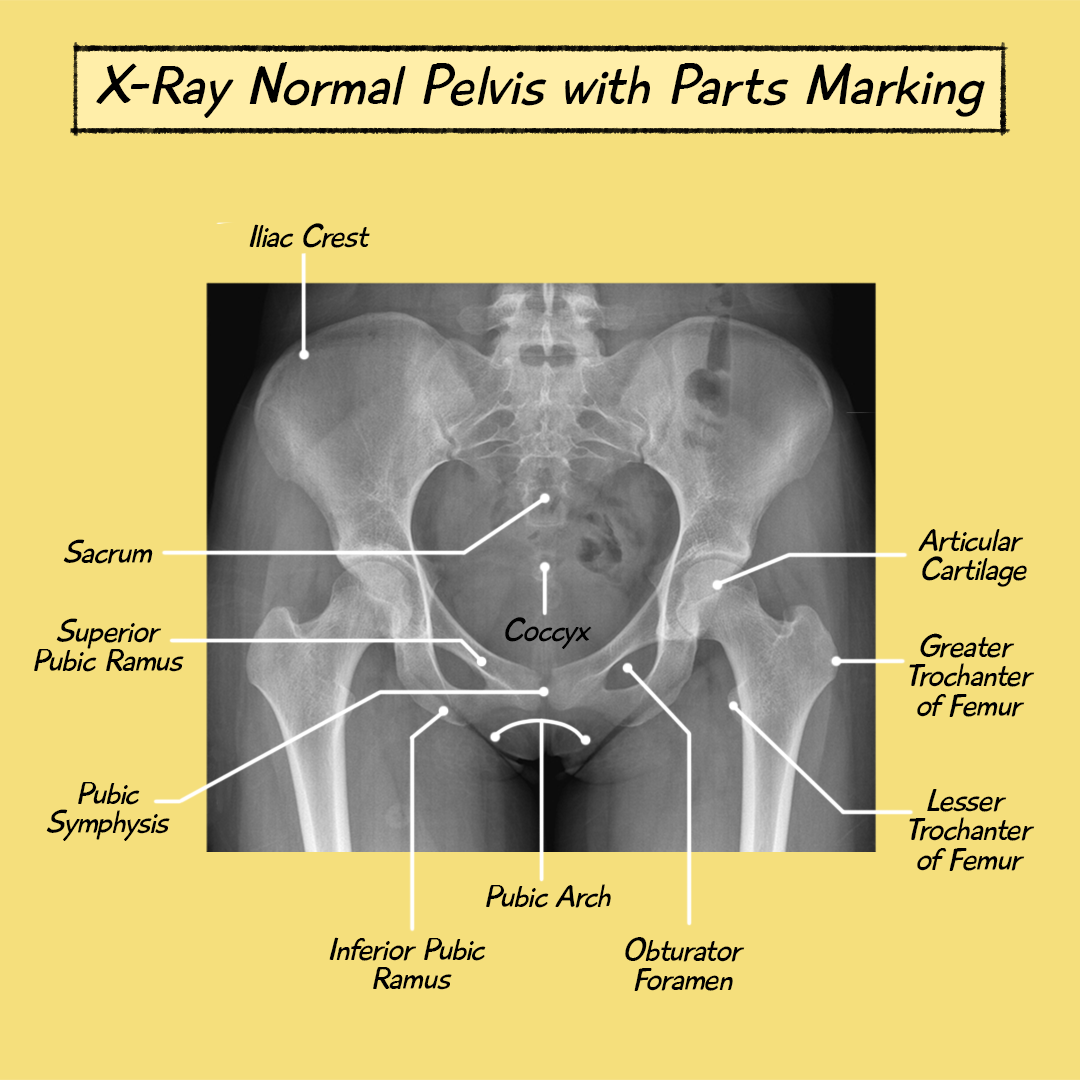
X-rays:
Anteroposterior (AP) view: The AP view is the standard initial radiograph for evaluating the pelvis.
It provides a general overview of the pelvic ring and can identify many fractures.



https://cdn.geckomed.ai/resources/7230f820-a585-11ef-b112-6f5929a3a4bf
Inlet view: The inlet view is obtained with the X-ray beam angled 45 degrees caudally.
It helps to assess the anterior-posterior displacement of the pelvic ring and identify fractures of the sacrum and posterior ilium.
Outlet view: The outlet view is obtained with the X-ray beam angled 45 degrees cephalad.
It helps to assess the vertical displacement of the hemipelvis and identify fractures of the ischium and pubic rami.
CT Scan:
Detailed Imaging: A CT scan provides detailed three-dimensional images of the pelvis and is essential for characterizing complex fractures and identifying associated injuries.
Surgical Planning: CT scans are valuable for surgical planning, allowing surgeons to visualize the fracture pattern and plan the optimal surgical approach.
Assessment of Soft Tissues: CT scans can also help to assess the extent of soft tissue injury and identify any hematomas or bleeding.
Other Imaging Modalities:
MRI: MRI may be useful in evaluating ligamentous injuries and assessing the extent of soft tissue damage.
Angiography: Angiography may be performed to identify the source of bleeding in patients with hemodynamic instability.
Prompt and appropriate management of pelvic fractures is essential to minimize complications and improve patient outcomes.
Management of Pelvic Fractures
The management of pelvic fractures requires a multidisciplinary approach involving trauma surgeons, orthopedic surgeons, intensivists, and rehabilitation specialists.
The goals of treatment are to control hemorrhage, stabilize the pelvis, relieve pain, prevent complications, and restore function.
Initial Management
The initial management of a pelvic fracture follows the principles of Advanced Trauma Life Support (ATLS).
Airway, Breathing, and Circulation (ABCs): Ensure a patent airway, adequate breathing, and circulatory support.
Address any life-threatening injuries first.
https://cdn.geckomed.ai/resources/08ffc8fb-30ec-4fea-ab7f-0acf83f1b8be
https://cdn.geckomed.ai/resources/7ccbf862-3d97-48fd-acb3-7866b331bef3
https://cdn.geckomed.ai/resources/0258a000-ecb6-4ec6-bbd4-f192720593af
https://cdn.geckomed.ai/resources/0d7ecfc4-c73c-4347-a8b5-89466bda7d6e
https://cdn.geckomed.ai/resources/0b7f2413-7c0e-4050-987d-3a3874ddd8ba
Hemorrhage Control:
- Pelvic Binders: A pelvic binder is a wide band that is applied around the pelvis to reduce pelvic volume and tamponade bleeding. It is a crucial first step in controlling hemorrhage in patients with suspected pelvic fractures.

- External Fixation: In unstable fractures, external fixation can be applied to stabilize the pelvis and reduce bleeding. External fixation involves placing pins into the iliac bones and connecting them to an external frame.
- Angiography/Embolization: If bleeding persists despite pelvic binder and external fixation, angiography can be used to identify the source of bleeding and embolize (block) the blood vessel. This is a minimally invasive procedure that can be life-saving in patients with uncontrolled pelvic hemorrhage.
https://cdn.geckomed.ai/resources/0405f8aa-93a8-4833-9c47-bf0da15fe64e
- Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA): In cases of severe, life-threatening hemorrhage, REBOA may be considered. This involves placing a balloon catheter into the aorta to temporarily occlude blood flow to the lower extremities, allowing time for resuscitation and definitive hemorrhage control.
https://cdn.geckomed.ai/resources/5d617088-940b-4ec5-a15c-d05a9aee31fa
- Pain Management: Provide adequate pain relief with intravenous analgesics. Pain control is essential for patient comfort and can also help to reduce physiological stress.
- Fluid Resuscitation: Administer intravenous fluids to maintain adequate blood pressure and perfusion. Monitor the patient’s vital signs and urine output closely.
The definitive treatment of a pelvic fracture depends on the type and severity of the fracture, the patient’s overall condition, and the presence of associated injuries.
Complications
Pelvic fractures are associated with a high risk of complications, both early and late.
Early Complications:
- Hemorrhage: Ongoing bleeding can be life-threatening, requiring aggressive resuscitation and hemorrhage control measures.
- Infection: Infection can occur at the surgical site, pin sites, or in the pelvis. Antibiotics and surgical debridement may be necessary.
https://cdn.geckomed.ai/resources/d92e9eff-af77-4ab4-b2d5-b514242e9513
- Thromboembolic Events: Pelvic fractures increase the risk of deep vein thrombosis (DVT) and pulmonary embolism (PE). Prophylactic anticoagulation is often recommended.
- Neurovascular Injury: Nerves and blood vessels in the pelvis can be injured during the injury or surgery. This can lead to numbness, weakness, or paralysis of the legs.
- Respiratory Complications: Patients with pelvic fractures may be at risk of respiratory complications, such as pneumonia and acute respiratory distress syndrome (ARDS), particularly if they have associated chest injuries or require prolonged immobility.
- Urinary Tract Infections: Urinary tract infections can occur due to urinary catheterization or bladder injury.
Gastrointestinal Complications: Gastrointestinal complications, such as ileus and constipation, can occur due to immobility and pain medications.