Intertrochanteric fractures represent a significant public health concern, particularly among the elderly population.
These fractures, occurring in the proximal femur, a crucial weight-bearing bone, often lead to significant morbidity, mortality, and healthcare costs.
This article provides a detailed exploration of intertrochanteric fractures, encompassing their definition, epidemiology, anatomical considerations, mechanisms of injury, clinical presentation, diagnostic approaches, management strategies, potential complications, and rehabilitation protocols.
The information presented here aims to equip medical students with a comprehensive understanding of this common orthopedic injury.
What is an Intertrochanteric Fracture?
An intertrochanteric fracture is a break in the femur that occurs in the region between the greater trochanter and the lesser trochanter.
These two prominent bony landmarks serve as critical attachment sites for major muscles involved in hip movement and stability.
The intertrochanteric region is particularly susceptible to fractures due to its anatomical structure and the significant biomechanical forces it experiences during weight-bearing activities.
Epidemiology
Intertrochanteric fractures predominantly affect older adults, with a marked increase in incidence among individuals over 65 years of age.
This heightened susceptibility in the elderly population is largely attributed to age-related bone loss and the prevalence of osteoporosis.
Osteoporosis, a condition characterized by decreased bone density and microarchitectural deterioration, weakens bones, making them more prone to fractures.
Women, particularly postmenopausal women, are at a higher risk due to the accelerated bone loss associated with estrogen deficiency.
Anatomy and Classification
Relevant Anatomy
Understanding the anatomy of the proximal femur is crucial for comprehending the mechanics of intertrochanteric fractures and their management.
The proximal femur comprises the femoral head, neck, and shaft.
- Femoral Head: This rounded portion articulates with the acetabulum of the pelvis to form the hip joint, enabling a wide range of motion.
- Femoral Neck: This connects the femoral head to the shaft and is a common site for fractures, especially in older adults.
- Greater Trochanter: This large, palpable bony prominence on the lateral side of the proximal femur serves as the attachment site for several muscles, including the gluteus medius and minimus, which are crucial for hip abduction and stability.
- Lesser Trochanter: This smaller prominence located medially and posteriorly provides attachment for the iliopsoas muscle, a primary hip flexor.
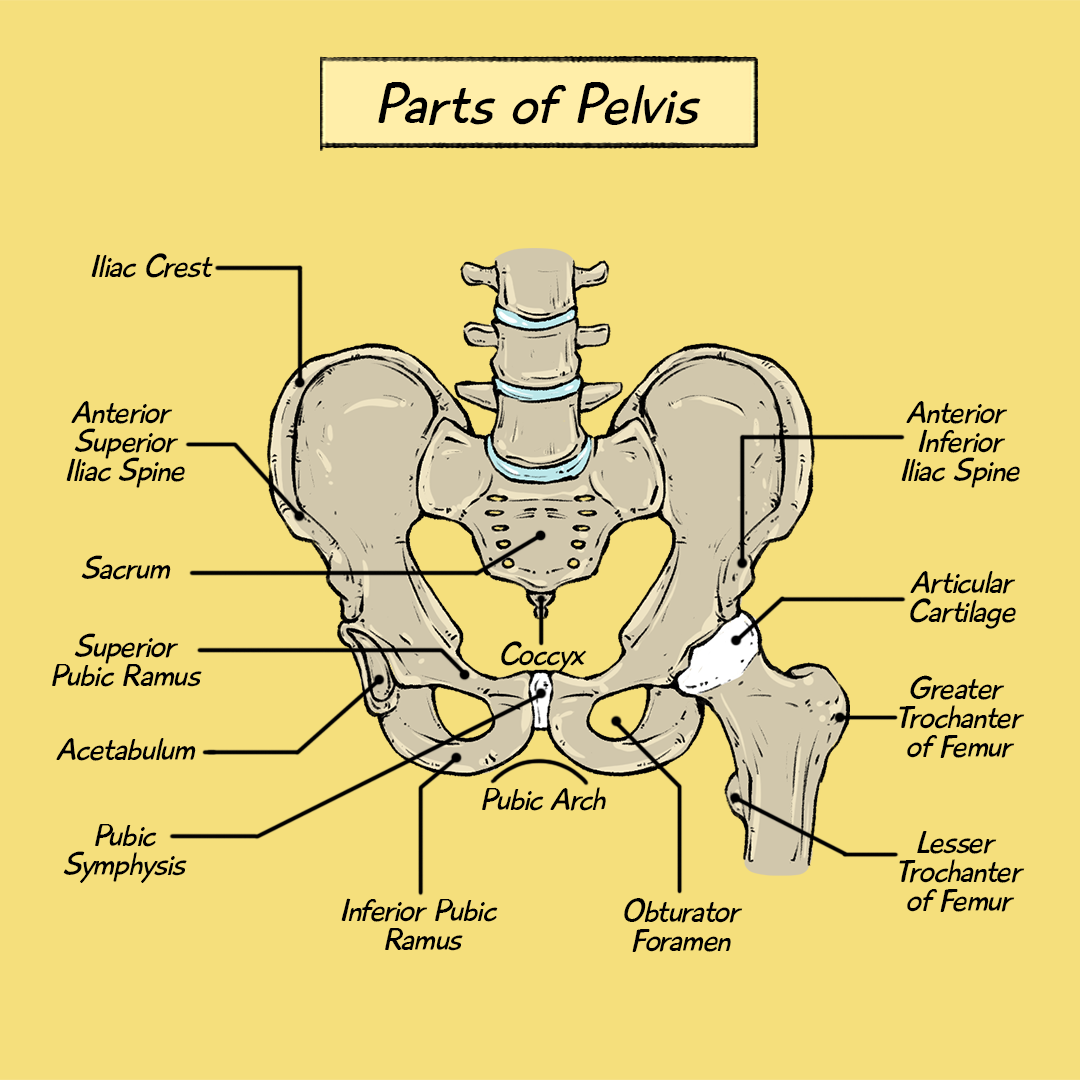
The intertrochanteric region lies between these two trochanters and is characterized by trabecular bone, a spongy type of bone tissue that is more susceptible to fractures than the denser cortical bone found in the femoral shaft.
Now, let’s examine how these fractures typically occur.
Intertrochanteric Fracture: Mechanism of Injury
Most intertrochanteric fractures result from low-energy falls, such as tripping or stumbling.
Common Causes
Intertrochanteric fractures typically result from low-energy trauma, most commonly a fall from standing height or a minor stumble.
In older individuals with osteoporosis or other underlying bone conditions, even seemingly trivial falls can generate sufficient force to cause a fracture.
Direct impact to the hip, such as in a motor vehicle accident or a fall from a significant height, can also lead to intertrochanteric fractures.
These high-energy injuries often result in more complex and comminuted fracture patterns.
Pathological fractures can occur in the intertrochanteric region due to pre-existing conditions that weaken the bone, such as metastatic tumors, primary bone tumors, or infections.
In these cases, the fracture may occur with minimal or no trauma.
Risk Factors
Several factors contribute to an increased risk of intertrochanteric fractures:
- Advanced Age: Age-related bone loss and decreased bone strength are major risk factors.
- Osteoporosis: This condition significantly weakens bones, making them more susceptible to fractures.
- Female Gender: Women have a higher risk due to hormonal changes associated with menopause.
- Underlying Medical Conditions: Certain medical conditions, such as rheumatoid arthritis, endocrine disorders, and neurological conditions, can affect bone health and increase fracture risk.
- Medications: Some medications, including corticosteroids, certain antidepressants, and proton pump inhibitors, can contribute to bone loss and increase fracture risk.
- Fall Risk: Factors that increase the risk of falls, such as impaired balance, muscle weakness, cognitive impairment, and environmental hazards, also increase the risk of intertrochanteric fractures.
- Nutritional Deficiencies: Inadequate intake of calcium and vitamin D can contribute to poor bone health.
- Smoking and Excessive Alcohol Consumption: These lifestyle factors can negatively impact bone density and increase fracture risk.
Understanding the clinical presentation and diagnostic methods is crucial for proper management.
Intertrochanteric Fracture: Clinical Presentation and Diagnosis
Patients with intertrochanteric fractures commonly present with severe hip pain, inability to bear weight, and shortening of the affected leg.
Symptoms
Patients with an intertrochanteric fracture typically present with a characteristic constellation of symptoms:
- Hip Pain: Severe pain in the hip or groin area is a hallmark symptom. The pain is often exacerbated by movement or attempts to bear weight.
- Inability to Bear Weight: Patients are usually unable to stand or walk on the affected leg due to pain and instability.
- Shortening and External Rotation of the Leg: The injured leg may appear shorter than the unaffected leg and rotated outward. This deformity is caused by the muscle forces acting on the fracture fragments.
- Swelling and Bruising: Swelling and bruising may be present around the hip and thigh area.
Physical Examination
A comprehensive physical examination is essential to assess the injury, evaluate the patient’s overall condition, and identify any associated injuries. The examination should include:
- Inspection: Observe the patient’s posture, gait (if possible), and any obvious deformities or signs of injury.
- Palpation: Gently palpate the hip and thigh area to assess for tenderness, swelling, and crepitus (a grating sensation caused by bone fragments rubbing against each other).
- Range of Motion: Evaluate the patient’s active and passive range of motion of the hip joint, noting any limitations or pain.
Neurovascular Assessment: Carefully assess the neurovascular status of the affected limb, including:
- Sensation: Test for sensation in the leg and foot using light touch and pinprick.
- Motor Function: Assess the strength of key muscle groups in the leg and foot.
- Pulses: Palpate the femoral, popliteal, dorsalis pedis, and posterior tibial pulses to ensure adequate blood flow.
- Capillary Refill: Assess capillary refill in the toes to evaluate peripheral circulation.
- Assessment for Associated Injuries: Examine the patient for other injuries that may have occurred during the fall or trauma, such as head injuries, spinal injuries, or fractures in other areas.
Imaging
Imaging studies play a crucial role in confirming the diagnosis, classifying the fracture, and guiding treatment planning.
X-rays: Anteroposterior (AP) and lateral views of the hip are standard radiographic images obtained to visualize the fracture.
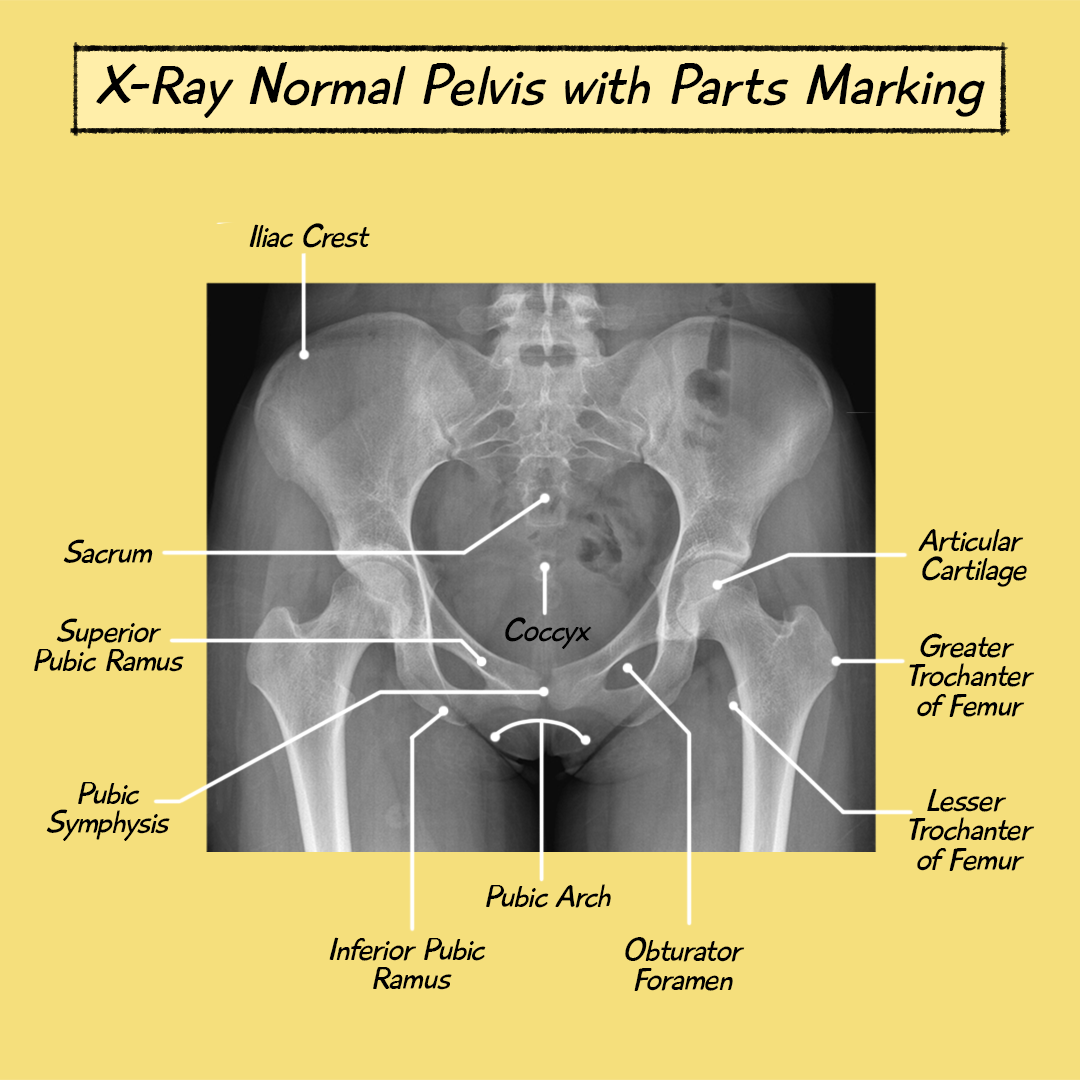
These images allow for assessment of the fracture location, pattern, displacement, and comminution.
CT Scan: A CT scan may be indicated for complex fractures or when the X-ray findings are inconclusive. CT provides detailed three-dimensional images that can help assess the extent of comminution, identify intra-articular involvement, and aid in pre-operative planning.
MRI: MRI is not routinely used in the initial evaluation of intertrochanteric fractures.
However, it may be helpful in certain cases, such as suspected occult fractures (fractures not visible on X-ray) or to evaluate for associated soft tissue injuries.
Management
The management of intertrochanteric fractures aims to achieve several key goals:
- Pain Relief: Effective pain management is crucial to ensure patient comfort and facilitate early mobilization.
- Restoration of Anatomical Alignment: Accurate reduction and alignment of the fracture fragments are essential for optimal healing and functional outcomes.
- Stable Fixation: Surgical fixation aims to stabilize the fracture, allowing for early mobilization and weight-bearing.
- Early Mobilization: Early mobilization is critical to prevent complications associated with prolonged bed rest, such as deep vein thrombosis, pulmonary embolism, pneumonia, and pressure ulcers. It also promotes faster recovery and improves functional outcomes.
- Prevention of Complications: Prompt diagnosis and appropriate treatment can help minimize the risk of complications associated with intertrochanteric fractures.
Non-Surgical Management
Non-operative management, primarily consisting of traction and bed rest, has a very limited role in the treatment of intertrochanteric fractures.
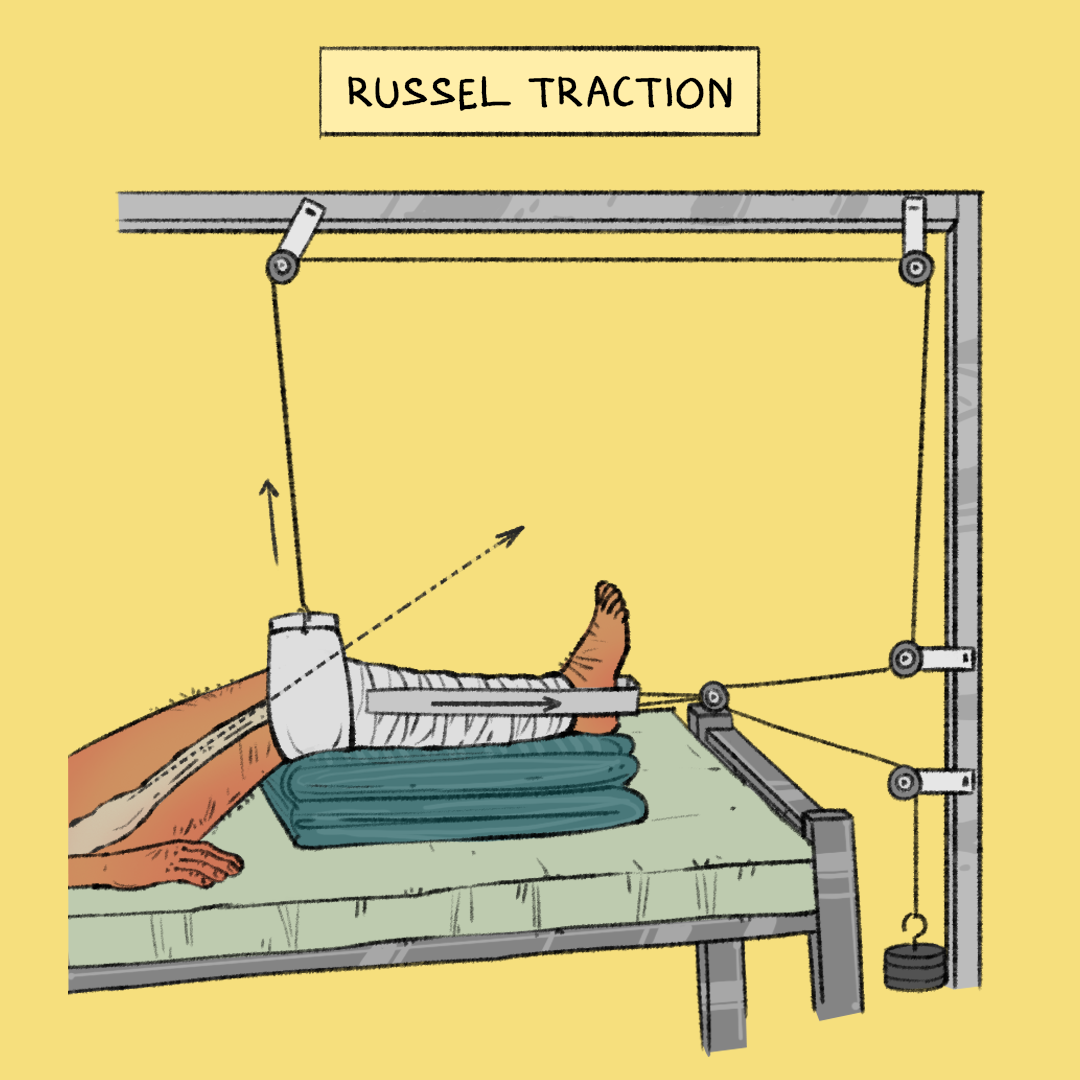

It may be considered only in rare cases where patients are deemed medically unfit for surgery due to severe comorbidities or high anesthetic risk.
In cases where the fracture is stable and non-displaced, Russell’s traction can be employed to maintain limb alignment and reduce muscle spasms, providing a period of initial immobilization and pain relief.
Derotation boots may also be utilized in conjunction with traction to control external rotation of the affected limb, further preventing displacement and promoting healing in minimally displaced fractures.
However, prolonged immobilization associated with non-surgical management can lead to significant complications and is generally not recommended.
Surgical Management
Surgical intervention is the mainstay of treatment for most intertrochanteric fractures.
The goals of surgery are to achieve stable fixation of the fracture, facilitate early mobilization, and restore function.
Types of Surgical Procedures
The choice of surgical procedure depends on several factors, including the fracture pattern, the patient’s bone quality, the presence of any comorbidities, and the surgeon’s experience and preference.
The two main surgical approaches are:
Extramedullary Fixation: This technique involves stabilizing the fracture with a plate and screws placed on the outside of the femur.
Commonly used implants for extramedullary fixation include:
Dynamic Hip Screw (DHS): This device consists of a large lag screw that is inserted into the femoral head and a side plate that is attached to the femoral shaft.
The lag screw slides within the barrel of the side plate, allowing for controlled collapse of the fracture fragments during the healing process.


DHS is often preferred for stable and simple fracture patterns.
Sliding Hip Screw: Similar to DHS, this device allows for controlled collapse and is suitable for stable fractures.
Intramedullary Fixation: This technique involves inserting a nail into the medullary canal (hollow center) of the femur.

https://cdn.geckomed.ai/resources/ac7006e0-37a1-11ef-bedb-f5604d06e805
Intramedullary nails provide strong fixation and allow for earlier weight-bearing.
They are particularly useful for unstable, comminuted, and reverse obliquity fractures.